Plantar Fasciitis: Symptoms, Common Causes & Treatments
Plantar fasciitis is inflammation of the plantar fascia, an area of your foot that connects your heel bone to your toes. What causes it and how is it treated?
6 minute read Plantar fasciitis is a common cause of heel pain that normally affects people between 40 and 60 years of age. It accounts for between 11 and 15% of foot problems requiring treatment and affects between 4 and 7% of people in the UK. Around one in ten people will develop plantar fasciitis during their lifetime.
What is plantar fasciitis?
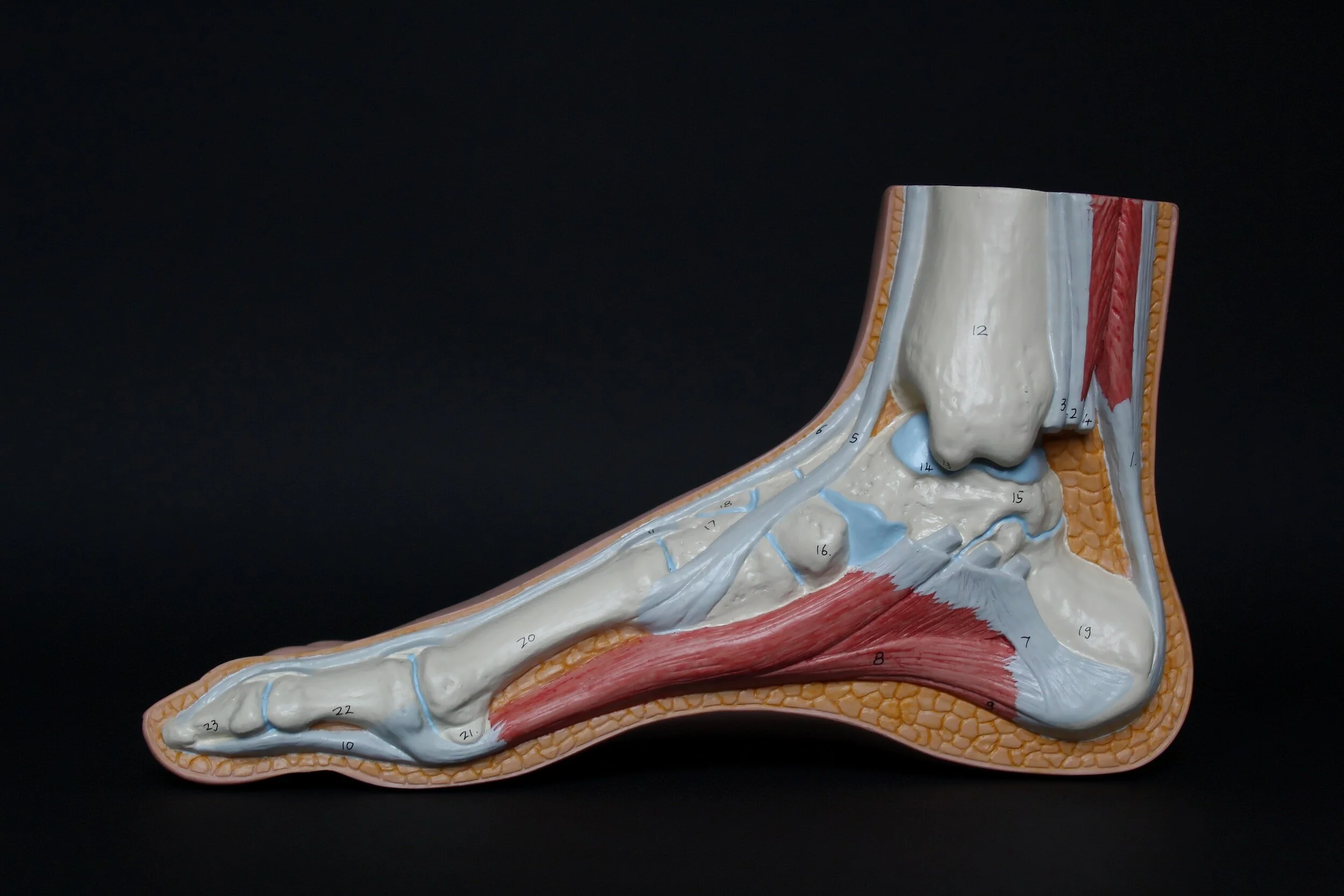
Plantar fasciitis is a condition where the plantar fascia becomes inflamed. The plantar fascia is a tough band of fibrous tissue that runs along the sole of the foot between the heel bone and the base of the toes.
The plantar fascia connects the bones in your foot together and helps support the arch of your foot. It also plays an important role in the mechanics of walking.
What are the symptoms of plantar fasciitis?
The main symptom of plantar fasciitis is pain around the heel. This can be a dull ache or a sharp stabbing pain and is usually worse after sleeping or resting. Pain may temporarily improve with exercise.
Other symptoms may include:
An aching or burning pain in the sole of your foot
Heel stiffness and swelling
Difficulty raising your toes off the floor
What causes plantar fasciitis?
Plantar fasciitis is caused by damage or irritation to the plantar fascia. Repeated stress and tension on the plantar fascia can cause small tears that may result in long-term irritation over time.
You may have a higher risk of developing plantar fasciitis if you:
Are aged 40 to 60
Have a job where you are on your feet all day
Exercise on a hard surface
Have recently increased your activity level
Exercise without warming up properly
Regularly wear shoes that don’t properly support or cushion your feet
Regularly walk or stand barefoot
Have a foot abnormality like high arches or flat feet
You walk with your feet excessively turned inwards (excessive pronation)
Have a health condition such as obesity, lupus, or rheumatoid arthritis
Are pregnant
When to see a doctor
Make an appointment to see your GP if:
You have severe pain that prevents you from doing normal activities
Your pain hasn’t improved after two weeks of home treatment
Your pain is getting worse or keeps coming back
You have other symptoms like numbness or tingling
You have diabetes
How is plantar fasciitis diagnosed?
Plantar fasciitis is diagnosed using a combination of your symptoms, medical history, and a physical examination of your foot.
Sometimes, your doctor may order tests such as a blood test or imaging tests like an X-ray, CT, or MRI scan to check for underlying health problems or rule out a different diagnosis.
Treatment for plantar fasciitis
Plantar fasciitis often gets better with home treatments.
Some things you can do to treat plantar fasciitis yourself include:
Rest your affected foot
Elevate your foot on a stool as much as possible
Apply an ice pack or a bag of frozen peas wrapped in a towel or cloth for up to 20 minutes every two to three hours
Wear shoes that support your foot arch and cushion your heels
Practise gentle stretching exercises for plantar fasciitis
Choose non-weight-bearing exercise like swimming
Take over-the-counter painkillers like paracetamol and ibuprofen
Lose weight if necessary
Avoid standing and walking for long periods
Avoid wearing shoes that don’t support your feet like high heels, flip-flops, tight, pointy, or backless shoes
Avoid walking barefoot on hard surfaces
Devices for plantar fasciitis
There are many products on the market such as socks, night splints, and orthotic insoles for plantar fasciitis and many people find them helpful. Talk to your pharmacist, GP, physiotherapist, or podiatrist about which device may be most suitable for you.
If your plantar fasciitis doesn’t improve after a couple of weeks of home treatments, your GP may refer you to a specialist.
Further treatment for plantar fasciitis may include:
Physiotherapy
A physiotherapist can teach you exercises to help stretch the plantar fascia and Achilles tendon and improve strength in your lower leg muscles.
Podiatry (chiropody)
A podiatrist can help relieve symptoms of plantar fasciitis and reduce the risk of it returning by strapping the affected area and advising you about supportive footwear and insoles.
Steroid injections
A steroid injection into the plantar fascia may be used to treat plantar fasciitis if other medications such as ibuprofen haven’t worked. Steroids work by reducing inflammation and swelling, and the effects usually last for several weeks.
Extracorporeal shockwave therapy
This is a procedure where shockwaves (low-energy sound waves) are passed through the skin to the plantar fascia. They work by increasing blood flow to the area, which helps to speed up the body’s healing process.
Shockwave therapies are commonly used across many parts of the human body to increase blood flow.
Surgery
In very rare cases, if other treatments haven’t worked, surgery called a plantar fasciectomy may be recommended to treat plantar fasciitis. Surgery involves cutting and releasing the fascia from the heel bone to decrease tension in the area.
Plantar Fasciitis: FAQs
How long does it take to recover from plantar fasciitis?
Recovery from plantar fasciitis can be slow and may take anywhere from a few months to over a year. Most people recover in between six and twelve months.
Is walking good for plantar fasciitis?
Walking after periods of rest may improve symptoms of plantar fasciitis by helping to stretch the ligament, but in time, walking may cause further inflammation and make your symptoms worse.
When walking, always wear the correct footwear or orthotics and avoid walking on hard surfaces.
How can I stop my plantar fasciitis from coming back?
It may not always be possible to prevent plantar fasciitis from coming back, but some things you can do to reduce your risk of the condition returning include:
Choose low-impact exercise such as gentle walking or swimming
Wear a night splint
Wash and moisturise your feet daily to prevent hard skin build-up
Wear shoes or orthotics that support your arch and heels
Apply ice packs and stretch your feet every morning
Can you cure plantar fasciitis?
With self-treatment and preventative measures, plantar fasciitis normally goes away completely and is considered cured.
Summary
Plantar fasciitis is one of the most common causes of heel pain, especially in people between 40 and 60 years of age. The condition usually improves with self-treatment, but in some cases may require further treatment such as physiotherapy, podiatry, or rarely, surgery.
If you have symptoms of plantar fasciitis that are not getting better with home treatments, make an appointment with your GP. Both NHS and private doctors will be able to diagnose this condition.
For more information about heel pain, including plantar fasciitis, watch this short video: